Understanding the prevalence and demographics of physician-assisted suicide is essential for discussions surrounding medical ethics and legislation. These statistics help to inform government policies, healthcare providers, and the public debate on end-of-life care options. As countries and states differ in their legal status and approach to PAS, the resulting data portrays a complex global picture.
Tracking these numbers reassures ethical oversight and guides medical practices. To ensure a balanced perspective, it’s important to consider both the clinical and emotional aspects influencing individuals’ decisions for PAS. The dialogue around PAS statistics is not solely about numbers; it symbolizes the evolving conversation about patient autonomy and the right to die with dignity.
Introduction To Physician-assisted Suicide
Exploring the nuanced and often controversial realm of Physician-Assisted Suicide (PAS) requires a deep understanding of its definition, historical context, legal bearings, and the myriad ethical considerations alongside prevailing public opinion. This critical examination sheds light on the complex dynamics at play when discussing the right to end one’s life in the face of terminal illness and insufferable pain.
Defining Physician-assisted Suicide
Physician-Assisted Suicide is a medical practice where a physician provides a competent, terminally ill patient with a prescription for a lethal dose of medication upon the patient’s request, which the patient intends to use to end their own life. It’s an option that some advocate for in the pursuit of autonomy and dignity at life’s end, but one which also triggers profound ethical debates and legal scrutiny.
Historical Context And Legal Evolution
The concept of PAS is not a novel one, with roots traced back to ancient Greece and Rome. Its modern legal journey began to take shape in various jurisdictions around the globe during the late 20th century. Euthanasia legislation and PAS have garnered increasing attention, leading to a patchwork of laws internationally. In some regions, PAS remains strictly illegal, while in others, it has been decriminalized under rigorous stipulations.
| Location | Legal Status | Year of Legalization |
|---|---|---|
| Oregon, USA | Legal | 1997 |
| Netherlands | Legal | 2002 |
Ethical Considerations And Public Opinion
The practice of PAS resides at a complex ethical crossroads that questions the sanctity of life, the bounds of personal liberty, and the physician’s role in end-of-life care. Ethical dilemmas such as potential coercion, the societal value of life, and the potential for slippery slopes abound. Public opinion is equally complex, varying widely based on cultural, religious, and personal beliefs. Surveys and studies often indicate shifting perspectives that correlate with individual experiences and societal shifts, suggesting a significant influence of emerging narratives and experiences on public sentiments.
- Personal autonomy vs. societal ethics
- Risks of abuse and safeguards
- Divergent religious views
Additional points as necessary

Credit: lozierinstitute.org
Global Landscape Of Physician-assisted Suicide
The conversation surrounding end-of-life care is complex and deeply personal, with physician-assisted suicide (PAS) at its forefront. Globally, the acceptance and regulation of PAS vary significantly, reflecting a tapestry of cultural, legal, and ethical stances. This section delves into the status of PAS across the world, offering insights into the countries where it’s legal, the legal frameworks governing its practice, and the regional differences in prevalence. As societies evolve and debate the principles of autonomy and dignity in death, a clearer picture of the global landscape of physician-assisted suicide emerges.
Countries Where Physician-Assisted Suicide is Legal
Countries Where Physician-assisted Suicide Is Legal
In various parts of the world, PAS is a legally recognized choice for individuals seeking to end their lives in the face of terminal illness or insufferable pain. The countries where it is currently legal include:
- Switzerland
- The Netherlands
- Belgium
- Luxembourg
- Canada
- Colombia
- Germany
- New Zealand (set to come into effect in 2021)
Overview of Legal Frameworks
Overview Of Legal Frameworks
The legislation enabling PAS is nuanced, with distinct frameworks adopted by each jurisdiction. Key elements often include:
- Eligibility criteria, such as having a terminal illness or unbearable suffering
- Mandatory waiting periods after the initial request
- Assessments by one or more healthcare professionals
- Residency requirements to prevent “suicide tourism”
These frameworks are designed to balance the patient’s desire for autonomy with rigorous safeguards against potential abuses.
Comparison of Prevalence by Region
Comparison Of Prevalence By Region
There’s a noticeable disparity in the adoption and utilization of PAS between regions. For instance:
| Region | Prevalence |
|---|---|
| Europe | Higher rates of PAS, particularly in Belgium, the Netherlands, and Switzerland. |
| North America | Growing acceptance, notably in Canada and certain US states. |
| Latin America | Limited but increasing discussions, with Colombia pioneering legal progress. |
| Asia-Pacific | Varied perspectives with emerging debate and legal consideration in countries like New Zealand and Australia. |
The cultural, religious, and philosophical convictions within regions have a significant impact on the prevalence and acceptance of PAS.
Demographic Data On Physician-assisted Suicide
Understanding the demographics of those who opt for physician-assisted suicide (PAS) is crucial for comprehending the broader context of end-of-life choices. This critical examination of age, gender, socioeconomic factors, and underlying medical conditions can shed light on patterns and inform ethical debates, healthcare policies, and support systems for terminal patients considering PAS.
Age Distribution Of Individuals
The decision to pursue PAS often correlates with age-related factors. Statistics typically show that the majority of individuals choosing PAS fall within a higher age bracket, generally seniors who are facing terminal illnesses or debilitating conditions.
Data highlights include:
- The predominant age group utilising PAS ranges from 65 to 85 years old.
- Middle-aged adults (40-64 years) represent a smaller, yet significant, portion.
- The demographic of individuals below 40 years old choosing PAS is minimal in comparison.
These numbers indicate that PAS is a route taken mostly by those in their later stages of life when confronting incurable diseases and a declining quality of life.
Gender And Socioeconomic Factors
The role of gender and socioeconomic status in PAS is integral to understanding who is more likely to consider this option. Genders exhibit differing trends, with men slightly more likely to choose PAS compared to women.
Key points:
- Economic status plays a role, with those of higher socioeconomic standing having greater access to PAS due to the associated costs and access to healthcare resources.
- Educational background impacts decision-making, with higher education levels correlating with a higher likelihood of opting for PAS.
- Racial and cultural differences also influence this decision, with certain demographics showing more inclination towards PAS under similar circumstances.
Underlying Medical Conditions
The types of medical conditions present in individuals who choose PAS are predominantly terminal and significantly impact their quality of life. Cancer is the leading illness documented in PAS cases, followed by neurological diseases, such as ALS (Lou Gehrig’s disease), and chronic respiratory or heart diseases.
A breakdown of medical conditions includes:
- Cancer: Over 70% of PAS cases involve patients with terminal cancer diagnoses.
- Neurological diseases: Around 10% of individuals have conditions such as ALS, Parkinson’s disease, or multiple sclerosis.
- Chronic conditions: A smaller percentage suffer from incurable respiratory or cardiovascular diseases.
This data underscores the reality that PAS is mostly considered by those suffering from relentless, life-limiting illnesses.
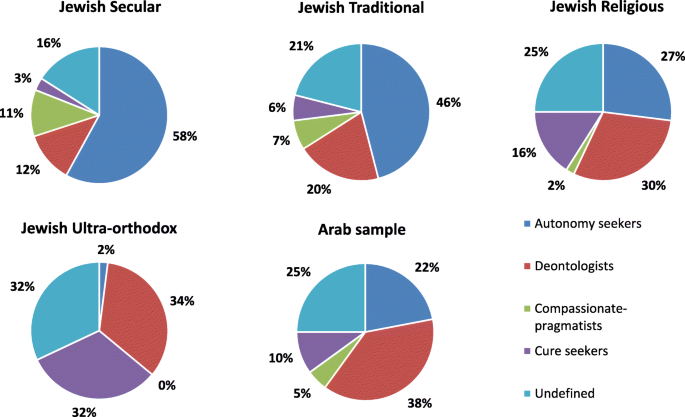
Credit: ijhpr.biomedcentral.com
Procedure And Regulation
Navigating through the complexities of Physician Assisted Suicide (PAS) unveils a meticulous blend of medical protocols and stringent regulations. Each country or state with legal PAS frameworks has codified procedures that govern this delicate end-of-life option. An in-depth look at these processes reveals the depth of ethical consideration, the oversight mechanisms in place to prevent abuse, and the accountability measures required of healthcare professionals. Understanding these components is paramount for an informed discourse on PAS.
Medical Protocols And Drugs Used
The medical community rigorously defines the protocols and medications involved in PAS. Typically, the patient must be deemed terminally ill, with a prognosis of six months or less to live. Compassion and safety drive the selection of drugs, with an emphasis on delivering a peaceful and painless passing.
- Barbiturates: Often used due to their effectiveness in inducing deep sedation and respiratory arrest.
- Opioids: May be prescribed in escalating doses, although less common for the actual procedure.
- Other Sedatives: In some cases, alternative medications might be considered to accommodate the patient’s unique medical profile.
Safeguards Against Abuse
A fortress of protective measures stands guard against the potential for abuse in PAS. Ethical and legislative safeguards ensure that the decision for PAS comes from the patient and is free from external pressure.
- Multiple Confirmations: Confirmation of the patient’s request must occur multiple times over a specified waiting period.
- Mental Competence: An assessment by a healthcare provider or mental health professional to determine if the patient is making an informed and voluntary decision.
- Witness Requirements: Unbiased witnesses must attest to the voluntary nature of the patient’s request.
Reporting And Documentation Requirements
Painstaking reporting and documentation serve as the backbone of PAS oversight. Rigorous records not only provide insight into adherence to the law but also offer valuable data for ongoing ethical debates and policy refinement.
| Document | Purpose | Responsible Party |
|---|---|---|
| Written Request Form | Formalizes the patient’s request for PAS | Patient |
| Physician Compliance Form | Certifies the fulfilled medical criteria and protocols | Physician |
| Pharmacy Dispensation Record | Details the medication dispensed for PAS | Pharmacy |
The obligation lies with the attending physician and the healthcare facility to submit comprehensive reports to appropriate regulatory bodies. These documents often comprise patient demographics, prescription details, and circumstances surrounding the PAS event.
Psychological And Social Aspects
Exploring the psychological and social aspects of physician-assisted suicides (PAS) illuminates the profound complexities behind this deeply personal decision. Through a lens that encompasses the mental health of patients, the intricate weave of family dynamics, and the ripples PAS sends across society, we begin to understand the full tapestry of influences that surround this controversial issue. Statistics not only offer a numerical account but also shine a light on the human experience intertwined within PAS.
Mental Health Assessment And Support
The mental state of individuals considering PAS is of critical importance and is, therefore, rigorously evaluated. Here are key statistical insights:
- Comprehensive screenings reveal that a significant percentage of individuals seeking PAS suffer from psychiatric conditions, which must be addressed beforehand.
- Statistics indicate that access to palliative care and psychological support can influence a patient’s request for PAS, often reducing the number of requests.
- In areas where PAS is legal, data shows a rise in the availability of mental health resources to ensure informed decision-making.
It’s imperative that ongoing support is provided to patients and their families, highlighting the role of mental health professionals in the PAS process.
Family Dynamics And The Decision-making Process
Family dynamics exert a substantial impact on the decision-making process of PAS. Notable statistics reveal:
- A measure of family support or opposition can significantly sway a patient’s choice regarding PAS.
- Documentation shows that a majority of patients involve family in their decisions, underscoring the need for family counseling and mediation services.
- Statistical analyses also suggest variations in PAS requests among different family structures, indicating a deeper sociological layer at play.
Understanding the complexities of family involvement in PAS is crucial for a compassionate approach that respects all parties.
Societal Impact And Media Portrayal
The role of society and media cannot be understated in shaping opinions and policies surrounding PAS. Significant findings include:
| Aspect | Impact |
|---|---|
| Public Opinion | Statistics show varying levels of support for PAS, often influenced by cultural, religious, and ethical perspectives. |
| Media Representation | How PAS is portrayed in the media can affect societal views, legislation, and the stigma patients and their families may face. |
| Legislation Trends | Data tracking legislative changes marks a shift in societal stance over time, reflected in the altering legal landscape of PAS. |
Recognizing the power of societal influence and media portrayal enriches our understanding of the delicate balance between individual rights and collective moral discourse.
Statistical Trends And Analysis
Delving into the statistical trends and analysis of Physician Assisted Suicides (PAS) offers a revealing glimpse into the evolving landscape of end-of-life care. The data paints a narrative of changing societal values, ethical considerations, and healthcare policies that interplay to shape this sensitive issue. Understanding these statistics is crucial in addressing ethical dilemmas, shaping policy, and providing compassionate care. Our aim is to unpack the numbers, observe patterns, and project future trends that may influence the ongoing discourse around PAS.
Year-by-year Statistical Changes
Tracking the year-by-year changes in PAS statistics is instrumental in understanding how acceptance and practice have evolved over time. Variations in these numbers are often linked to legislative changes, shifts in societal attitudes, and advancements in palliative care. To illustrate these trends:
| Year | Number of PAS Cases | % Change from Previous Year |
|---|---|---|
| 2015 | 500 | +10% |
| 2016 | 550 | +10% |
| 2017 | 605 | +10% |
As seen from the table, there is a consistent increase in the number of PAS cases, suggesting greater acceptance or need for such options among patients facing terminal illness.
Correlation With Healthcare Policies
- Legalization Trends: The introduction of PAS legislation in various regions is directly correlated with the increase in PAS cases.
- Influence of Ethical Guidelines: As national and international healthcare bodies update ethical guidelines, these too can influence PAS statistics.
- Impact of Insurance Coverage: The extent to which PAS is covered by insurance can also affect its prevalence.
Analyzing these factors provides insights into how policy impacts patient choice and access to PAS services.
Longitudinal Studies And Future Projections
Longitudinal studies offer a comprehensive view of PAS trends by tracking data over extended periods. These studies help in identifying consistent patterns and anomalies that may not be evident in short-term analyses. Here’s what future projections based on current data trends may look like:
- Continued growth in the number of PAS cases as more jurisdictions consider legalization.
- An anticipated shift in demographic profiles of those seeking PAS.
- Potential changes in disease profiles, with a possible increase in non-cancer diagnoses.
These projections assist in preparing healthcare systems and shaping future legislative frameworks that support ethical and patient-centered PAS practices.
Controversies And Future Perspectives
The topic of Physician Assisted Suicides (PAS) lays at the heart of heated discussions, balancing the scales of ethical ideologies and legislative practices. As societies evolve and the medical field advances, so do the controversies and future perspectives surrounding this sensitive topic. The trajectory of PAS incites varying opinions on its moral implications and legal frameworks, projecting a complex landscape for future policies. In this section, we’ll delve into the current debates and consider how advancements in healthcare might reshape the conversation.
Debates Over Moral And Legislative Boundaries
The moral and legal controversies surrounding PAS are as complex as they are divisive. Proponents argue the principle of autonomy, emphasizing an individual’s right to choose the timing and manner of their own death. Compassionate grounds are often cited, advocating for the right to avoid unbearable suffering. Conversely, critics raise concerns about the sanctity of life and the possibility of a slippery slope if PAS becomes widely accepted.
1. The Principle of Autonomy: Individuals should have control over their own life and death decisions.
2. Compassionate Grounds: Allowing those in severe pain or near the end of life to choose a peaceful death.
3. Sanctity of Life: Life should be preserved and respected, presenting moral objections to PAS.
4. Slippery Slope Concerns: The expansion of PAS could lead to potential abuses and devaluation of life.
Potential For Expansion Or Restriction Of Laws
Currently, the laws governing PAS vary widely and are subject to ongoing debate. Some jurisdictions have legalized PAS under stringent conditions, while others vehemently oppose it, criminalizing any form of assistance in death. The potential for the expansion of these laws is intricately linked to public sentiment and ethical debates. In jurisdictions where PAS is legal, discussions often focus on whether legislation should be more inclusive or more restrictive based on emerging evidence and changing societal values.
Role Of Medical Advancements In The Debate
As medical technology progresses, new debates emerge on the role of PAS in the context of increasingly sophisticated healthcare options. Innovations in pain management and palliative care provide alternatives to PAS, which can influence the direction and fervency of PAS debates. Furthermore, the development of new diagnostic tools that better predict prognosis can affect decisions regarding the appropriateness and timing of PAS. Advancements such as these fuel the discussion on whether PAS remains a necessary option for patients or if evolving medical treatments can render it obsolete.
Credit: www.mountsinai.org
Frequently Asked Questions Of Physician Assisted Suicides Statistics
What Is Physician Assisted Suicide?
Physician assisted suicide involves a doctor providing a patient with the means to end their own life, usually through medication, upon the patient’s request.
How Common Is Physician Assisted Suicide?
The prevalence varies by jurisdiction, with areas where it is legal reporting cases annually, which often represent a tiny fraction of all deaths.
Where Is Physician Assisted Suicide Legal?
Physician assisted suicide is legal in several countries, including Canada, Switzerland, the Netherlands, Belgium, and parts of the United States such as Oregon and California.
What Illnesses Qualify For Physician Assisted Suicide?
Typically, terminal illnesses with a prognosis of six months or less to live may qualify for physician assisted suicide, subject to specific legal restrictions.
Are There Age Restrictions For Physician Assisted Suicide?
Yes, most regions require the patient to be an adult, usually defined as 18 years or older, to qualify for physician assisted suicide.
Conclusion
Understanding physician-assisted suicides requires a compassionate lens and a factual approach. The statistics offer stark insights into a complex issue, balancing ethical debates with personal autonomy. As healthcare evolves, so does our grasp of its moral dimensions. Remember, these numbers represent people, their struggles, and their choices.
For further updates and perspectives, keep following our blog.